The Case for Healthcare Innovation: Four Critical Shifts to Watch
CCV Investor Vayum Arora (WG26) outlines key inflection points in healthcare.
The healthcare ecosystem is at a pivotal moment. Four major forces — demographic, technological, cultural, and regulatory — are reshaping the global healthcare landscape, creating opportunities to address long-standing inefficiencies and catalyze innovation.
Here’s why now is a pivotal moment for investing in healthcare:
1. Demographic Shift: America is Getting Older
The global population is aging rapidly. In the U.S. alone, the proportion of adults aged 65 and older is projected to grow from 16% in 2020 to over 20% by 2030. Countries like Japan are already grappling with more extreme aging demographics, where nearly 30% of the population is over 65. Globally, we’re witnessing a pivotal moment in history: for the first time ever, the number of people in the US aged 65 and older will soon surpass the number of children under five.
This "Silver Tsunami" is driven by declining birth rates, longer life expectancy, and improved healthcare. With it comes a surge in age-related diseases — Alzheimer’s cases alone are projected to nearly double from 6.7 million today to 13 million by 2050. Alzheimer’s cases, for example, are expected to nearly double by 2050, from 6.7 million today to 13 million. The strain on caregivers and healthcare systems will only intensify, raising critical questions: who will deliver care, and how will it be funded?
Opportunities lie in scaling aging-in-place technologies, training a new generation of healthcare workers to address a rapidly aging patient base, and building integrated care models that better serve this growing elderly demographic. Innovators who address these challenges will define the next era of elder care.
2. Technological Shift: Data, Wearables, and Interoperability
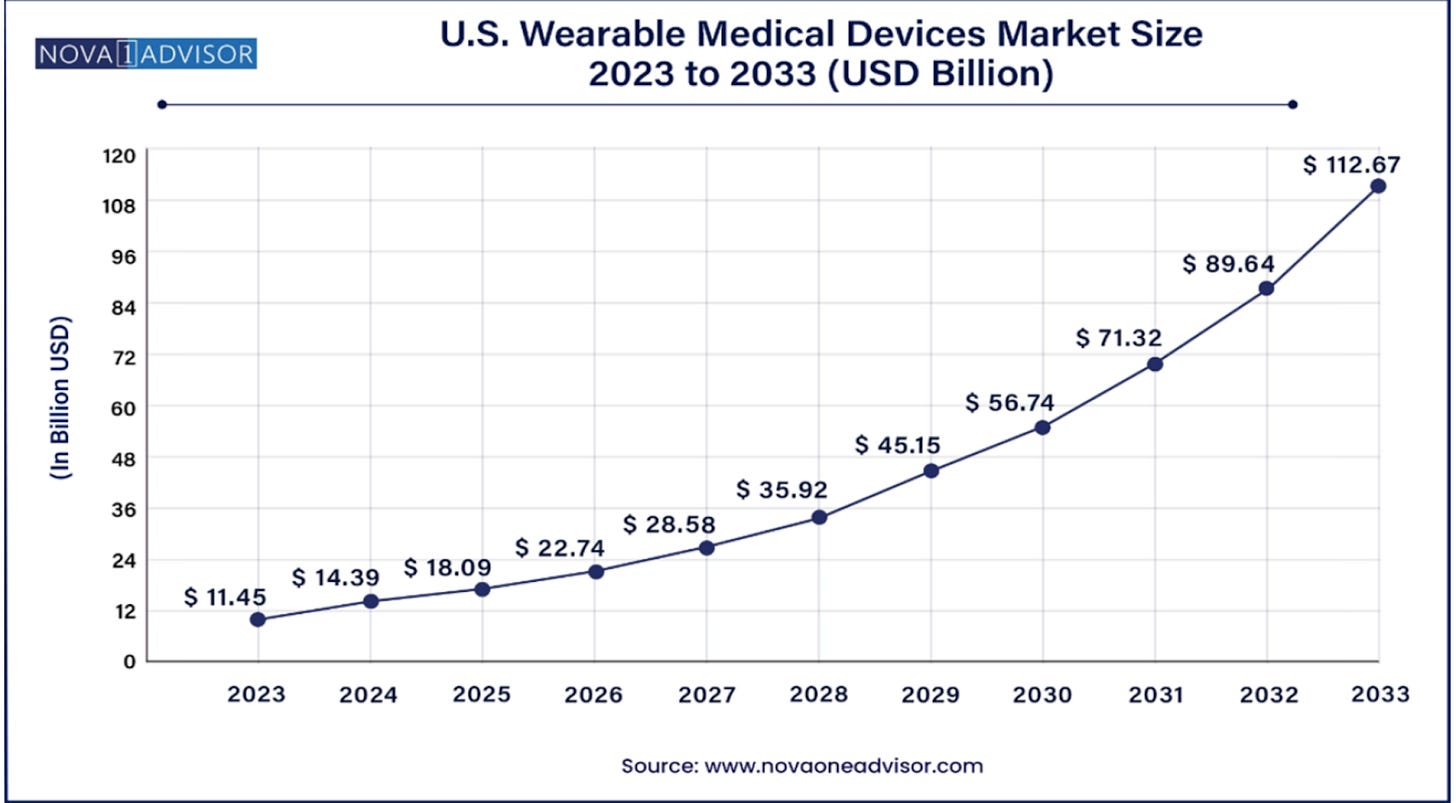
By 2025, healthcare data is expected to account for 36% of the world’s total data volume. This deluge of information is both a challenge and an opportunity. Wearables like the Apple Watch,, Whoop band, and Oura ring now track everything from heart rate variability to oxygen saturation levels. Over 30% of U.S. adults use these devices, yet much of this data remains locked within proprietary platforms, siloed from the broader healthcare system.
The lack of inter-device interoperability limits what wearables can actually do. With better integration, this data could identify early signs of conditions like heart disease or diabetes, enabling timely interventions. But most healthcare providers work with fragmented or incomplete datasets, missing critical opportunities for prevention and personalized care.
Platforms like Redox and Spike are working to bridge these gaps by integrating biosensor data with electronic health records (EHRs), unlocking the potential of medical diagnostic devices. The promise of interoperability is simple: connected systems mean actionable insights, which lead to better care. With healthcare data volumes exploding, making these connections isn’t just nice to have—it’s essential.
3. Cultural Shift: Obesity and GLP-1 Medications
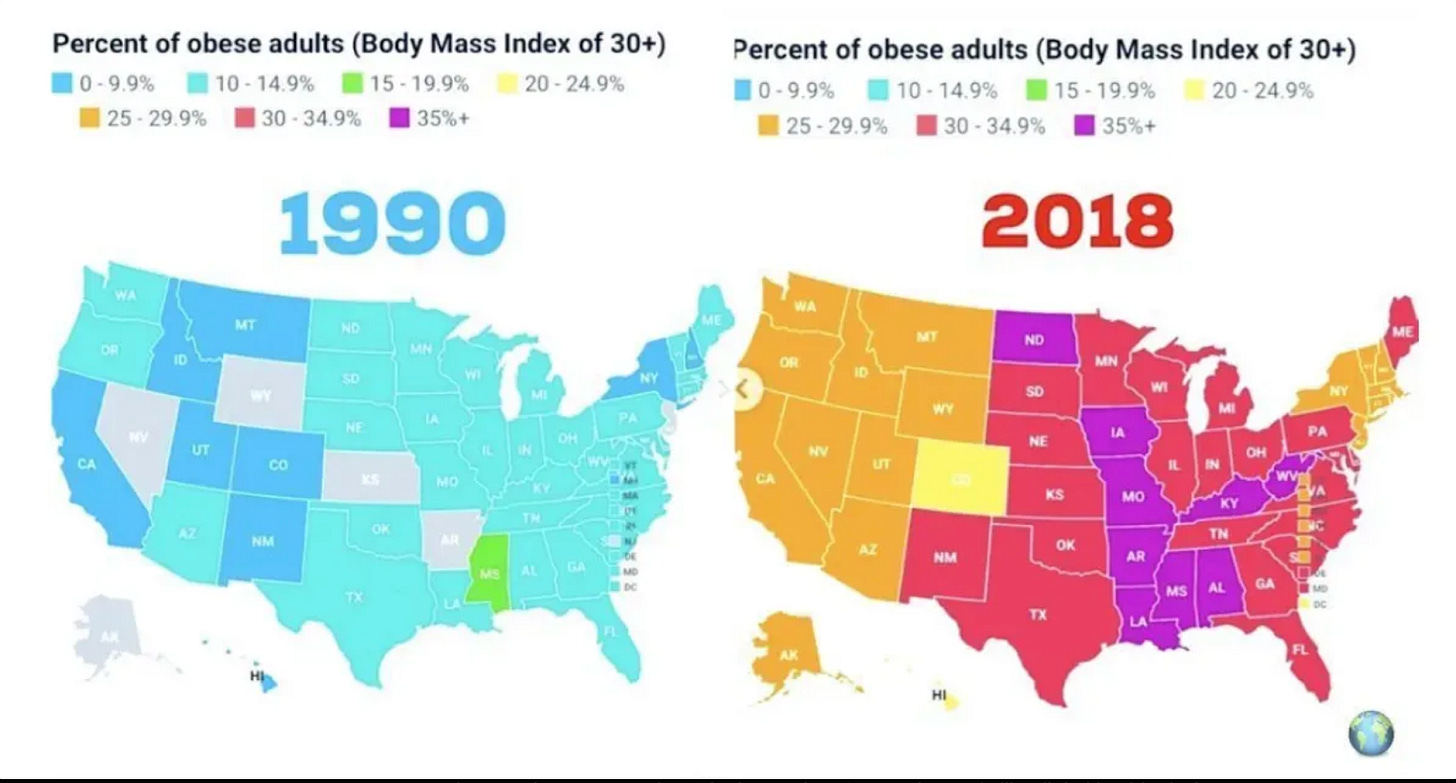
Obesity has become a defining health crisis, affecting over 40% of U.S. adults. Over the last two decades, rates have climbed significantly, exacerbating chronic diseases and driving up healthcare costs. Enter GLP-1 drugs like Ozempic and Wegovy, which represent breakthroughs in weight management that are able to deliver double-digit percentage weight loss for patients.
But GLP-1 medications aren’t a cure-all. Many patients regain weight after discontinuing these drugs, and their high cost — often exceeding $1,000 per month with limited insurance coverage — makes them inaccessible to much of the population. This underscores a broader issue: equitable access to long-term solutions for obesity and related chronic conditions.
These gaps in care open doors for innovation. Companion tools like digital health platforms, personalized nutrition programs, and behavior modification technologies could make weight loss treatments more effective and accessible. The line between clinical care and wellness is blurring, creating space for new approaches that go beyond prescriptions.
For more insights on these topics, check out The Gut Punch, a Wharton-founded deep-dive series on The Ozempic Era, exploring how our food system fueled the obesity crisis and the untold risks of weight loss drugs.
5. Regulatory Shift: A More Open Playing Field
Physician wait times in major cities are alarmingly high. Patients wait 52 days to see a physician in Boston and over 30 days here in Philadelphia. Similar delays exist nationwide. Behavioral health services are particularly strained, where delayed care often leads to adverse outcomes. The pandemic brought these inefficiencies into sharp focus, prompting temporary regulatory changes.
Temporary waivers in the Ryan Haight Act allowed telehealth providers to prescribe controlled substances without requiring in-person evaluations, drastically improving access to care for underserved populations. Similarly, state-level reforms like New York’s temporary practice permits for International Medical Graduates (IMGs) have helped address provider shortages in overburdened systems.
These changes reflect a system inching toward flexibility. Making these reforms permanent could create fertile ground for startups to expand telehealth services, optimize workflows, and build innovative care models that adapt to evolving demands.
4. Innovation is at a Breaking Point
The recent assassination of UnitedHealthcare CEO Brian Thompson shocked the nation, but it also exposed a deeper truth about the U.S. healthcare system: the American people are fed up. The public reaction to this event — ranging from outrage to unsettling support for the alleged shooter — reflects a growing frustration with a system that seems to prioritize profits over patients. Denied claims, unaffordable treatments, and endless delays have become the norm, leaving Americans frustrated and exhausted.
And the frustration feels warranted. The United States spends $4.1 trillion annually on healthcare—the equivalent of running the world’s fourth-largest economy—and yet our outcomes don’t match the investment. Chronic conditions eat up 90% of these costs, while misaligned incentives between payers and providers create inefficiencies that make accessing care harder than it should be. The result? Delayed treatments, worsening conditions, and a system that feels broken at its core.
Startups that are able to find ways to use innovation to address customers’ fundamental frustration with the U.S. healthcare system can achieve unprecedented growth while also solving real, high-priority problems felt by the American people.
The four transformative shifts explored —demographic, technological, cultural, and regulatory—are not just signals of systemic strain; they’re catalysts for action. The Luigi Mangione incident, though tragic, is a sobering reminder of the stakes. It underscores the urgent need to address systemic failures before they deepen further. For startups and changemakers, this is a moment to not only fix inefficiencies but also rebuild trust, prioritize equity, and create solutions that truly serve the people.
If you’re building in the space or have thoughts on the shifts reshaping healthcare, I’d love to connect!
You can reach Vayum on LinkedIn here. For more insights from our team, don’t forget to subscribe to Center City Ventures Insights on Substack — we’ll be back with more!